Highlights
- Macular degeneration is the leading cause of irreversible blindness in older adults, impacting daily life.
- Current treatments aim to slow progression and preserve vision, with promising therapies on the horizon.
Summary
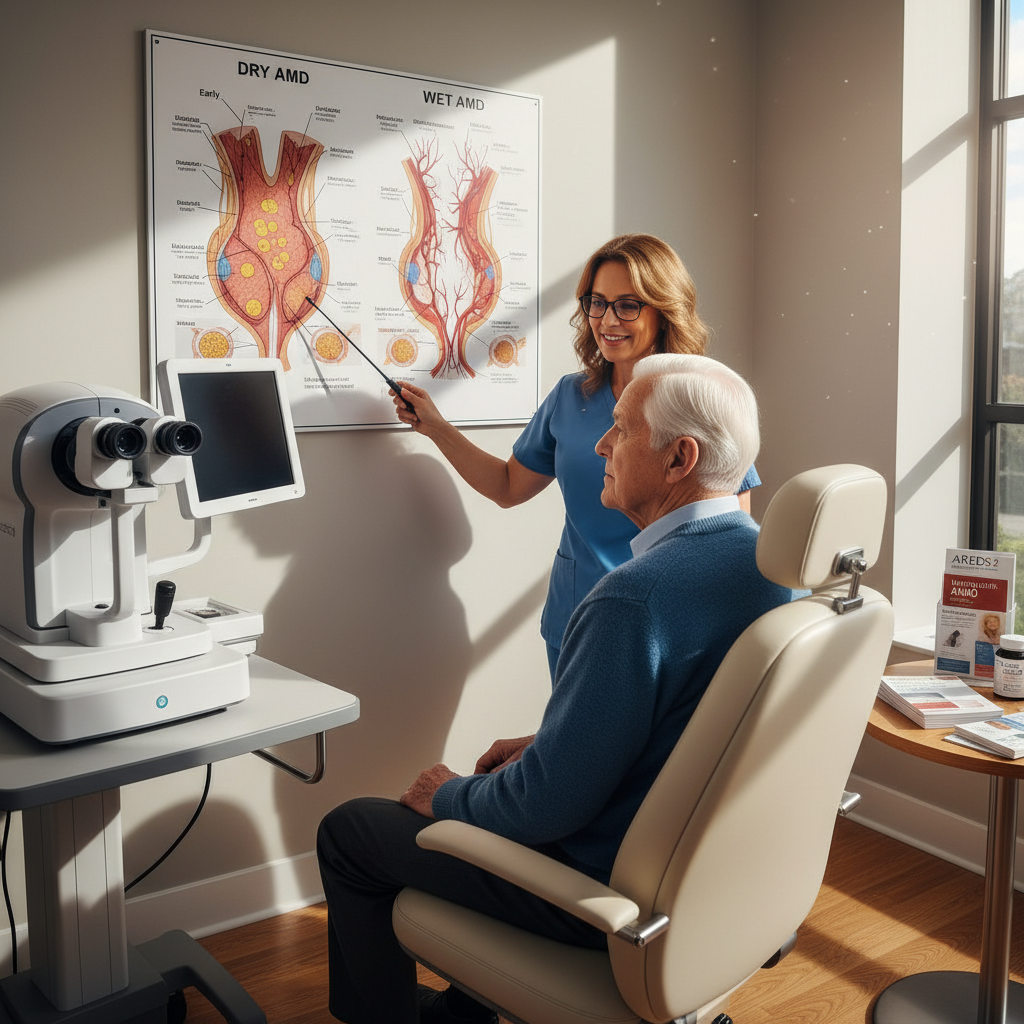
The Essential Guide to Macular Degeneration outlines macular degeneration, a progressive eye disease affecting the macula, the retina’s central area responsible for sharp vision. It is the leading cause of irreversible blindness in older adults in developed countries, impairing activities like reading and face recognition. The disease occurs mainly as dry (atrophic) AMD, involving gradual macular thinning and drusen accumulation, or wet (neovascular) AMD, marked by abnormal blood vessel growth causing rapid vision loss. Diagnosis involves eye exams and imaging, with treatments aiming to slow progression—nutritional supplements for dry AMD and anti-VEGF injections for wet AMD. New therapies, including complement inhibitors and gene therapy trials, offer hope for improved management. Coping strategies and rehabilitation support quality of life amid vision loss.
Anatomy and Function of the Macula
The macula is an oval, pigmented area near the retina’s center, about 5.5 mm in diameter, containing regions such as the fovea and foveola responsible for sharp central vision. Its yellow color comes from dietary carotenoids that protect against blue and UV light. The macula has the highest density of cone photoreceptors for detailed color vision, particularly in the fovea. Supporting structures like the Henle fiber layer and Muller glial cells maintain retinal function. Imaging advances like optical coherence tomography (OCT) help visualize macular anatomy and diagnose diseases.
Types, Classification, Causes, and Risk Factors
Age-related macular degeneration (AMD) has two main types: dry AMD, characterized by macular thinning and drusen deposits progressing to geographic atrophy, and wet AMD, involving abnormal blood vessel growth under the retina causing leakage and rapid vision loss. Classification systems incorporate anatomical, genetic, and environmental factors for risk assessment. AMD risk is influenced by genetics (notably complement system genes), age-related retinal changes, and lifestyle factors like smoking, diet, blood pressure, and obesity. While genetic testing is not routine, ongoing research explores gene therapy. Other risk factors include inflammation and systemic conditions. Preventive measures emphasize smoking cessation, healthy diet, and cardiovascular health.
Pathophysiology
AMD involves progressive degeneration of the macula. Dry AMD features drusen accumulation and retinal cell loss leading to geographic atrophy. Wet AMD results from choroidal neovascularization, causing fluid leakage, scarring, and rapid vision loss. Oxidative stress, immune dysregulation, and metabolic factors contribute to disease progression. The macula’s unique cellular structure and high metabolic demand make it vulnerable to damage.
Signs and Symptoms
Dry AMD often progresses slowly with early stages causing no symptoms, while intermediate stages may cause mild blurriness or difficulty in low light. Late dry AMD leads to geographic atrophy and central vision loss. Wet AMD causes rapid vision deterioration with symptoms like distorted or blurred central vision, dark spots, and difficulty with tasks requiring fine detail. Although total blindness is rare, central vision loss significantly affects daily activities. Regular monitoring using tools like the Amsler grid helps detect early changes.
Diagnosis
Early AMD is often asymptomatic but detectable via comprehensive eye exams, including pupil dilation and retinal imaging. Tests like the Amsler grid identify visual distortions. Diagnosis of wet AMD involves detecting choroidal neovascularization and retinal changes. High-resolution OCT imaging enhances detection and monitoring. Prompt diagnosis allows timely intervention to preserve vision.
Prevention and Risk Reduction
Prevention focuses on modifiable factors: quitting smoking, maintaining healthy weight, controlling blood pressure and cholesterol, and following a diet rich in antioxidants and carotenoids, such as the Mediterranean diet. Vitamin supplements based on AREDS2 are recommended for intermediate to advanced dry AMD. Awareness of risk factors guides preventive strategies.
Treatment
Treatment depends on AMD type and stage. Dry AMD has no cure but can be managed with AREDS2 supplements to slow progression. Recently approved complement inhibitors (Syfovre and Izervay) help slow geographic atrophy. Stem cell therapies are under investigation. Wet AMD treatment centers on anti-VEGF injections (e.g., aflibercept, ranibizumab) to inhibit abnormal vessels, with biosimilars expanding options. Emerging gene therapies aim to reduce injection frequency and provide durable effects. Low vision rehabilitation and assistive devices support functional vision. Regular monitoring is essential for timely treatment adjustments.
Impact on Daily Life and Coping Strategies
Macular degeneration impairs central vision, affecting reading, face recognition, and driving, leading to challenges in independence and social interaction. Emotional effects include anxiety and depression; some patients experience visual hallucinations (Charles Bonnet syndrome). Coping involves low vision rehabilitation, assistive technologies, support groups, and counseling, which improve quality of life. Emerging therapies, including implantable lenses and perceptual training, offer additional benefits.
Epidemiology
AMD is a leading cause of irreversible blindness, especially in people over 55 of European and North American descent. Prevalence is rising worldwide due to aging populations. Genetic variants significantly influence susceptibility, alongside lifestyle factors like smoking. Understanding epidemiology aids in risk prediction and prevention.
Research and Developments
Research has advanced treatments for AMD, supported by organizations like BrightFocus. Complement inhibitors offer new options for geographic atrophy. Anti-VEGF therapies remain central for wet AMD, with biosimilars improving access. Gene therapies in clinical trials promise longer-lasting effects. Genetic studies inform future personalized treatments, though routine genetic testing is not yet standard. Ongoing research aims to improve early detection and therapeutic outcomes.
The content is provided by Blake Sterling, Scopewires