Highlights
- Nasal polyps significantly impact quality of life, often requiring long-term management strategies.
- Emerging biologic therapies provide promising options for severe cases, though costs and side effects vary.
Summary
Nasal polyps are benign, painless growths from the nasal mucosa linked to chronic inflammation, often seen in chronic rhinosinusitis (CRS). They cause nasal obstruction, reduced smell, and facial pressure, impacting quality of life. Occurring worldwide, they often coexist with asthma, aspirin-exacerbated respiratory disease, and cystic fibrosis. Their formation involves genetic, environmental, and immune factors, especially type 2 inflammation. Diagnosis uses clinical evaluation, nasal endoscopy, and CT imaging. Treatment includes intranasal corticosteroids, oral steroids, surgery, and newer biologics targeting inflammation. Despite treatment advances, polyps often recur, requiring long-term management and ongoing research into targeted therapies.
Anatomy, Definition, and Clinical Presentation
The nasal passages, lined with mucous membranes, warm and filter inhaled air. Nasal polyps are soft growths from this lining, often due to chronic inflammation, obstructing airflow and impairing smell. They present with nasal blockage, rhinorrhea, facial pressure, and reduced smell. Physical exam and nasal endoscopy help identify polyps, which are usually painless and mobile. Polyps can obstruct sinus drainage, leading to infections and complications like orbital involvement. They commonly occur with chronic rhinosinusitis and systemic conditions such as cystic fibrosis and aspirin-exacerbated respiratory disease.
Epidemiology and Pathophysiology
Nasal polyps are linked to allergies, asthma, chronic sinus infections, aspirin sensitivity, and cystic fibrosis. Genetic factors, including over 150 variants in immune and inflammatory pathways, contribute to susceptibility. Environmental exposures and smoking may play roles. Pathophysiology involves chronic inflammation driven by immune responses, especially type 2 inflammation with cytokines IL-4, IL-5, and IL-13, leading to eosinophilic infiltration and tissue remodeling. Factors like Staphylococcus aureus exotoxins and microbiota imbalance exacerbate inflammation. Defects in epithelial barriers and genetic predisposition influence disease severity. Polyps can cause sinus obstruction, sleep apnea, and anosmia.
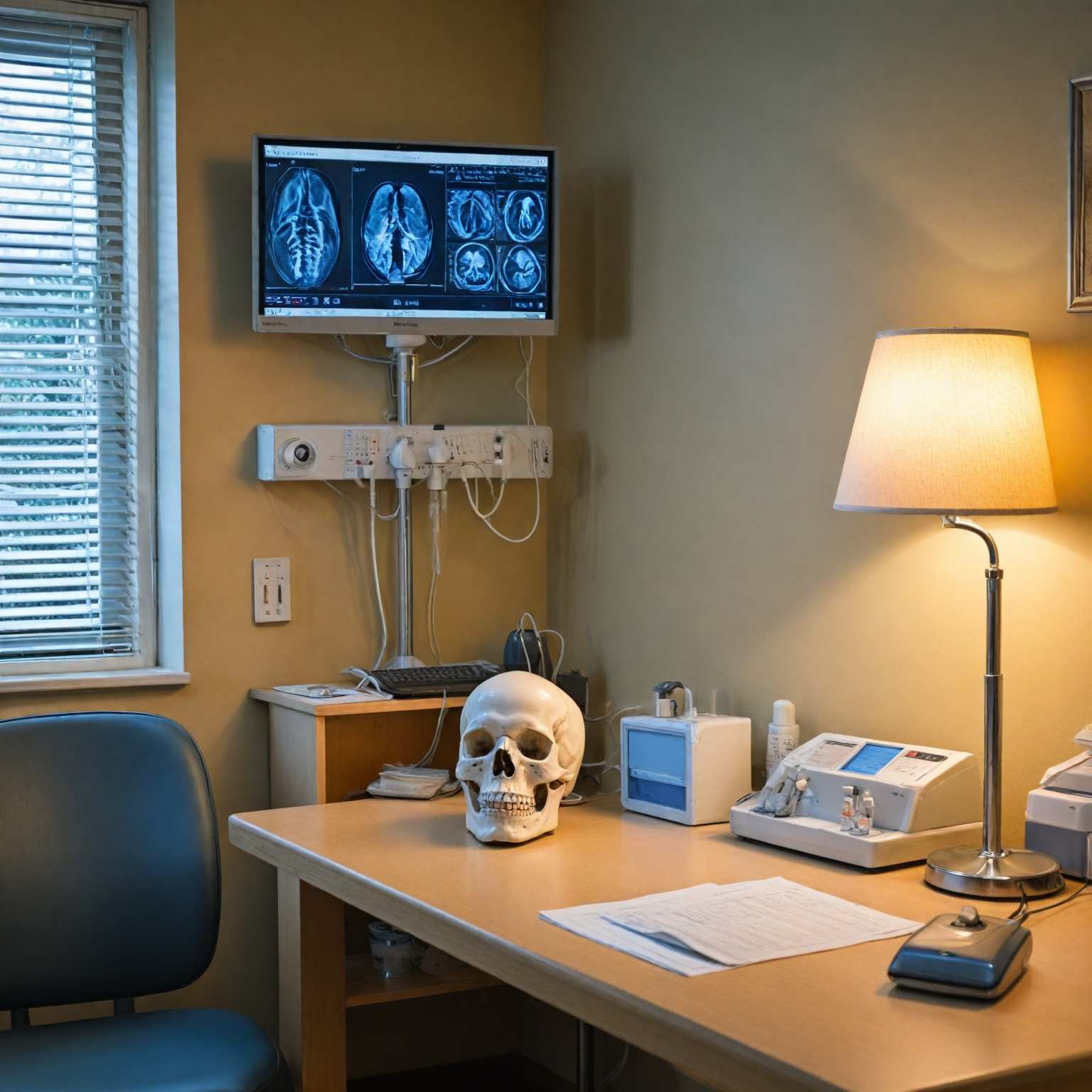
Diagnosis
Diagnosis depends on clinical history, physical exam, and nasal endoscopy to visualize polyps. CT scans assess disease extent, anatomical variations, and guide surgery, distinguishing polyps from tumors. MRI is reserved for suspected soft tissue or orbital involvement. Biopsy is rarely needed unless atypical features or malignancy are suspected.
Treatment and Management
Treatment aims to reduce polyp size, relieve symptoms, and prevent recurrence. First-line therapy is intranasal corticosteroids, which decrease inflammation and polyp size. Oral corticosteroids are used for moderate to severe cases or when rapid symptom relief is needed. Surgery is considered when medical therapy fails, with postoperative corticosteroids reducing recurrence risk. Biologic therapies, such as dupilumab, omalizumab, and mepolizumab, target specific inflammatory pathways and benefit patients with severe or recurrent disease but are costly and have potential side effects. Adjunct measures like nasal saline irrigation support symptom relief. Prevention includes avoiding environmental triggers and occupational exposures.
Complications and Prognosis
Complications include recurrent sinus infections, sleep apnea, nasal obstruction, and, rarely, orbital involvement. Nasal polyps often recur despite treatment, with 5-10% experiencing severe recurrence post-surgery. Long-term management and monitoring are essential. Biologics offer benefits for recurrent or refractory cases but have limitations due to side effects and cost. Genetic factors affect recurrence and treatment response, highlighting the need for individualized care.
Research and Future Directions
Research focuses on the genetic and molecular basis of nasal polyps, identifying numerous variants and microRNAs involved in inflammation and tissue remodeling. Biologic therapies targeting type 2 inflammation show promise but require further study on safety, cost-effectiveness, and long-term outcomes. Surgical techniques continue to improve, with adjunctive medical treatments reducing recurrence. Advanced imaging like MRI and cone beam CT may enhance diagnosis and management. Ongoing studies explore novel therapies, including NSAIDs, to inhibit polyp growth and improve patient outcomes.
The content is provided by Jordan Fields, Scopewires